ℹ️ This is the case information for the doctor.
Name
Amanda Davies
Age
32 years
Address
73 Drake Avenue
Social history
Marital Status: Married to Mark Davies, age 44.
Smoking: Does not smoke.
Alcohol: Does not drink.
Past history
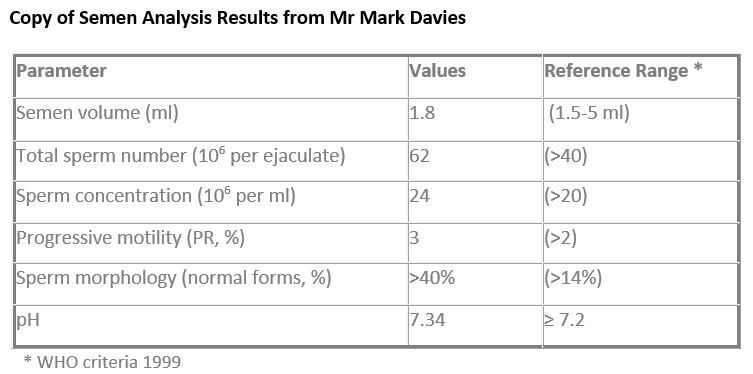
Investigation results
Medication
Booking note
Requests appointment for conception advice.
ℹ️ This is the information for the person role playing the patient.
Name
Amanda Davies
Age
32 years
Address
73 Drake Avenue
Social history
Marital Status: Married to Mark Davies, age 44.
Smoking: Does not smoke.
Alcohol: Does not drink.
Past history
Medication
Sorry to trouble you doctor but I wondered if you might be able to refer me to an infertility specialist… I also wondered if you can tell me the result of Mark’s semen test he had last week, you should have them back by now
Living situation: Recently moved into a new house with Mark. Wedding in 3 months (planning ceremony now).
Employment: Works at Sainsbury's as a checkout assistant.
Marital Status: Married to Mark Davies, age 44, estate agent.
Medication taken over the counter: Prenatal supplement: Pregnacare tablets (self-purchased, not prescribed).
General health: You are otherwise well, taking Pregnacare, and not on any other medication.
Gynae history
ℹ️ To mark data gathering & diagnosis select from the descriptors below.
Positive descriptors
Negative descriptors
Data gathering was systematic and targeted ensuring patient safety.
Data gathering was incomplete, lacking structure and focus.
Makes effective use of existing information and considers the wider context.
Fails to use the information provided or understand the wider context.
The presence or absence of relevant red flags was established.
Fails to assess key information necessary to determine risk.
Information gathered placed the problem in its psychosocial context.
The social and psychological impact of the problem was not adequately determined.
Relevant information was collected to place the undifferentiated problem in context and an appropriate differential diagnosis generated.
Inadequate information was collected to determine the likely cause of symptoms.
Revises hypotheses as necessary in light of additional information.
Rigid consulting with new information not adequately considered and integrated into the working diagnosis.
ℹ️ To mark clinical management & medical complexity select from the descriptors below.
Positive descriptors
Negative descriptors
Offers management options that are safe and appropriate:
Fails to provide appropriate and/or safe management choices:
Continuity of care is prioritised:
Ongoing care is uncoordinated:
Empowers self-care and independence:
Management fails to foster self-care and patient involvement:
Prescribes safely considering local and national guidance:
Unsafe prescribing ignoring best practice:
Practises holistically, promoting health, and safeguarding:
Fails to safeguard patient welfare:
Does not break Mark’s confidentiality:
Breaks Mark’s confidentiality:
ℹ️ To mark relating to others select from the descriptors below.
Positive descriptors
Negative descriptors
Explores the patient’s agenda, health beliefs and preferences:
Fails to recognise the patient’s agenda and impact of the problem:
Recognises what matters to the patient and works collaboratively to enhance patient care:
Fails to work with the patient to plan care:
Demonstrates flexibility of communication adapting to the patient and scenario:
Consults rigidly, providing generic explanations and management plans:
Respectfully challenges unhelpful health beliefs or behaviours:
(80% of women aged under 40 years conceive within 1 year, 90% within 2 years)
Fails to maintain a productive therapeutic relationship:
Checks the patient’s understanding of the consultation including any agreed plans:
Does not seek to confirm understanding:
Adapts thinking to overcome challenges, creating practical and effective solutions:
Fails to adjust thinking when faced with obstacles, leading to ineffective or impractical solutions:
ℹ️ Insights from the examiner
Start the consultation with open-ended questions to encourage Amanda to share her story. This both supports rapport and provides efficient data gathering.
"I can see this is really important to you. How things have been for you and Mark recently?"
Elicit the patients agenda early so you can focus in on what matters to her most.
Use focused questions to clarify timing, frequency of intercourse, prior contraceptive use, and any red flags (such as previous pelvic surgery, irregular periods, or known medical problems for either partner). Check what has already been tried (eg, timing ovulation, lifestyle measures, previous tests/investigations). Try to avoid untargeted questions that do not directly relate to the case.
"Have either of you had any investigations before, for example blood tests or hormone checks?"
Summarise as you go to check you are aligned to her agenda. This grounds the consultation, prevents backtracking, and supports structured, sequential data acquisition.
Clarify Amanda’s (and Mark's if known) current steps/prior investigations, to avoid repetition and respond proportionately.
You are aiming to have completed data gathering by minute 6-7 of the consultation so that you have adequate time to cover the management of the case.
Use clear, supportive language at Amanda's level of understanding. Acknowledge her anxieties.
"Trying for a baby can be a very emotional process, especially when things are taking longer than you expected."
Explain medical terms simply and with a positive frame:
"Fertility specialists usually work with couples who have been trying for a year or more, because the vast majority of couples will get pregnant within a year of trying"
Look for Amanda’s verbal and non-verbal cues regarding anxiety, frustration, embarrassment, or expectations about early referral and test results. For example;
“I can see this has been stressful and it’s really on your mind – how has it been affecting you and Mark?”
Address her expectations gently but honestly. If she appears more anxious if referral is not immediately offered, explore and validate this:
“That’s a very common reaction when things aren’t happening as quickly as hoped, but you’re certainly not alone. Can you tell me more about what you’ve found most difficult?”
Involve Amanda in setting realistic goals for today’s consultation, and the ongoing journey.
"What are you hoping we can achieve together today?"
"Would it help to know more about what to expect and when we would refer if it was needed?"
Ensure your questions progress logically: history of trying to conceive, menstrual and sexual history, medical/surgical history, stress impact, partner’s health. Acknowledge each answer to show active listening.
"Your periods sound regular, and you’re both healthy overall, which is reassuring..."
Ask about potential risk factors sensitively (eg, history of STIs, pelvic surgery, previous difficulties conceiving for either partner).
Infertility differentials in a woman with regular cycles, normal sexual frequency, and no red flags:
Amanda has no urgent red flags for early female investigation per NICE [NICE CG156]
Explore psychological, social and relationship impact to tailor support:
"You mentioned that this has been difficult for you and Mark. Can you tell me more about how you're both coping?"
This can help Amanda feel validated and informs your holistic management recommendations (eg, couple support/counselling).
Keep explanations brief, clear and relevant. Avoid jargon – especially about referral thresholds:
“Most couples will conceive within 12 months of trying. If it hasn’t happened by then, we can arrange further tests for both you and Mark. If you have any new symptoms, or if things change, we can always review things earlier.”
Share your clinical reasoning to keep her engaged and reduce anxiety:
"From what you’ve told me, there don’t seem to be obvious reasons for delay. National guidelines say to wait until 12 months, but I’ll outline exactly what we’ll do at that point, and what we would do sooner if anything changes."
Offer a range of strategies and advice in line with NICE guidance; explain pros and cons for each, and support patient-led decision-making:
If Amanda expects Mark’s result: Explain sensitively that by law you cannot provide partner’s results without their explicit consent (NICE, GMC confidentiality guidance). Offer joint appointment or for Mark to receive/collect his result directly.
Check Amanda’s understanding throughout:
"Does this all make sense so far? Is there anything unclear, or any concerns you’d like me to go over again?"
Check how she feels about the plan for review, and involve her in decisions for follow-up and support.
Personalise your plan based on Amanda’s relationship strain, emotional needs, and lack of red flags for early investigation:
"I know it must feel frustrating, but the good news is that everything you’ve mentioned is reassuring and in line with what we’d hope for at this stage. Can I suggest we make a follow-up appointment for five months’ time (to reach the 12 months), and earlier if anything changes? In the meantime, I can give you some leaflets and links for reliable advice and support."
References: